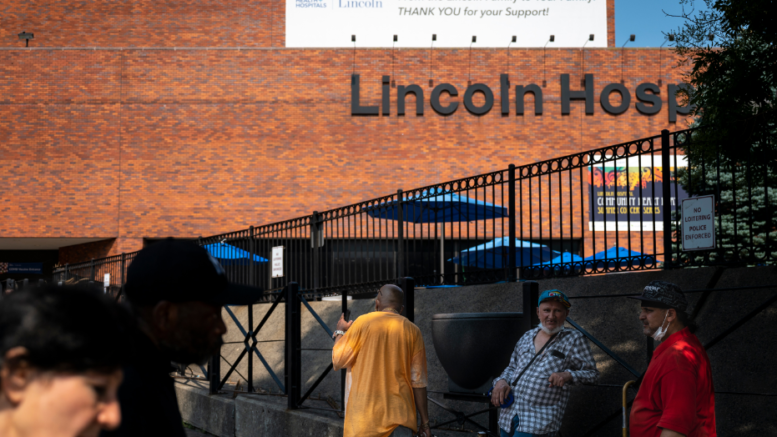
Some residents at the city-run Lincoln Hospital in The Bronx are in revolt over an allegedly “toxic culture” following the deaths of three medical trainees between August 2020 and April of this year.
The deaths came to public attention after an advocate for better working conditions for doctors and medical residents wrote a online column headlined: “Why Three MDs From One Hospital Died by Suicide Within 8 Months: Can We Stop This?”
On Wednesday, the website Medscape removed a version of that column after posting a response from two Lincoln Hospital officials that disputed some of the piece’s claims.
Hospital medical director Dr. Vihren Dimitrov and director of internal medicine Dr. Nehad Shabarek wrote: “We lost two residents to suicide. Though no less horrific, the third death was investigated and declared an accident by the police department.”
At least one of the doctors-in-training died by suicide, family members confirmed to THE CITY. Another perished in a drowning in Hawaii that witnesses said was accidental. THE CITY is withholding the deceased residents’ names at families’ requests.
All three came from overseas to complete their medical training at Lincoln and were residents at the public hospital’s Department of Internal Medicine, where some current and former employees describe a culture of bullying, harassment and dysfunction.
Treating COVID patients only added to existing stresses — which are especially intense for the international residents on work authorization visas signed for by hospital administrators, current and former employees said.
None of the current or former employees THE CITY spoke with were willing to have their names published, out of concern for professional consequences.
The 11-hospital NYC Health + Hospitals system currently hosts about 2,000 residents, 325 of them at Lincoln.
‘I Felt Horrible’
Ex-residents at Lincoln said they often chose not to report conflicts, or confront higher-ups because they feared losing their work permits. One graduate, who spoke with THE CITY on the condition of anonymity, said a top supervisor threatened to dismiss her — which would immediately end her ability to work in the U.S. — after a misunderstanding about scheduled time off.
“It’s so malignant and toxic,” the graduate said. “It’s a terrible, terrible, terrible place, which is why I felt horrible going to work. I’d feel sick, like actually physically sick, to go to work.”
In their column, Dimitrov and Shabarek wrote: “No resident has ever been threatened to have their visa canceled or withdrawn. Never.
“As for the allegations of ‘toxic culture’ at Lincoln — many of our graduates chose to stay on as attendings, serve the local community, and train new residents,” the Lincoln leaders added. “Out of the 67 attendings in our department, 24 are former graduates. They are being joined by another five graduates from this year’s graduating class. There is no better testament to how our graduates feel about our residency program, Department of Medicine, and Lincoln Hospital.”
Hospital residency programs, where medical school graduates receive training and prepare for specialties, are notoriously tough.
All U.S. graduates must do at least one year of training in internal medicine in programs like Lincoln’s, with additional years of training in specialties. Internists-in-training may do as many as three years of residency rounds in internal medicine.
The often grueling working conditions for residents have long been targets for reform. In the 1980s, a crusade by journalist Sidney Zion following the death of his 18-year-old daughter Libby while a tired resident napped led to some limits. Today, residents may work no more than 80 hours a week, averaged over four weeks, and no more than 24 hours on duty at a stretch, with certain exceptions.
The Committee for Interns and Residents, a union representing the state’s medical trainees, including those at Lincoln, is pushing for a strict 80-hour work week limit, “not as an average and including non-clinical tasks.”
‘I Would Not Like You’
The pressures of the sometimes life-and-death work — a core part of how hospitals deliver services to patients — have prompted calls for reform. At the Icahn School of Medicine at Mount Sinai in Manhattan, the suicides of two medical students in 2016, one of them during her residency, prompted a task force to evaluate changes to the institution’s culture.
Among its recommendations: expanding staff and trainee access to mental health specialists and opening a “hub” for well-being, The Wall Street Journal reported at the time.
A former Lincoln trainee who volunteered to colleaguesthat she was struggling emotionally told THE CITY that program leaders and even some fellow residentsscolded her as too soft for the job. When she and another resident became withdrawn under the strain, she added, fellow trainees and some of the leadership picked on them.
The other resident was one of the two who died by suicide, she said.
“I wanted to tell him, ‘Just hang in there, it’s going to be finished so soon,’” she said. “Because I was finishing up in a few months, and I wanted to tell him that but I never did. I could tell that he was bullied just like I was.”
“It was very much this sense of like, ‘Oh, we suffered when we were residents, or when we were in our first year, so now you have to suffer too,’” she said. The former resident added that other departments at Lincoln where she rotated didn’t have such issues.
Residents report to attending physicians and delegate certain tasks, like triaging and administering dosages, to nursing staff. But at the internal medicine program at Lincoln, miscommunication meant residents were often left on their own — and whenever something went wrong, they said, attending physicians blamed residents.
One graduate said she sees a PTSD specialist since leaving Lincoln. She said she was routinely bullied by other residents and “constantly” publicly excoriated by a supervisor who once told her, “If I were your friend, I would not like you.”
Support System Touted
The NYC Health + Hospitals system has measures in place to support medical staff in distress, said Chief Equality Officer Dr. Eric Wei.
In an interview with THE CITY, he pointed to the system’s Helping Healers Heal program, a mental health initiative designed to promote wellness on the job and help doctors cope with the loss of patients.
The program deploys social workers and mental health professionals, including psychiatrists, when a physician requests assistance. Since 2018 more than 1,000 medical workers have received peer-support training to prepare them to identify and assist colleagues in distress, according to Wei.
Wei said personnel from Helping Healers Heal, called H3 for short, immediately deployed to Lincoln in the aftermath of the deaths, sending grief counselors and other mental health aid to staff. But he acknowledged the program “is not meant to address suicide” — and said H+H officials are considering whether to change that going forward.
Wei also pointed to powerful structural barriers to doctors seeking mental health help while in training. State medical licensing agencies, he noted, ask applicants if they’ve ever received mental health services.
A 2018 study published in the The Journal of the American Academy of Psychiatry and the Law found that medical students who have received psychiatric treatment have “reduced prospects for residency placements.”
While the Americans with Disabilities Act prohibits discrimination on the basis of being diagnosed with or in treatment for a mental disorder, physician advocates and researchers say state medical boards often get away with it.
“What we’re trying to do is see if there’s more that we can do to destigmatize people asking for help. We’re fighting against decades, even centuries of this culture,” Wei said.
Services and a Ping-Pong Table
Lincoln Hospital took some measures to ease pressure on its doctors and residents
in the early months of the pandemic, when The Bronx was one of the hardest-hit areas in the world. The hospital’s psychiatry department pivoted to provide walk-in clinics on-site for medical staff to talk one-on-one, according to a hospital source.
But those clinics shut down in July 2020 once the hospital re-opened for elective treatment — not long before the first internal medicine resident at the hospital died suddenly in late August.
Lincoln hosted memorials at the hospital for each of the three deceased residents, opening the services to hospital staff and loved ones. After the first staff death, according to residents there at the time, hospital leadership installed a ping-pong table in a medical recreation room.
An H+H spokesperson said the move had already been in progress, after staff requested the table.
Still, current and former residents say management did little else to address morale issues, and forbade staff from discussing the deaths.
A spokesperson for H+H rejected those claims, stating that the agency provides free grief services to all employees regardless of the death they experienced.
Resident physicians at Lincoln, through their union, said in a statement to THE CITY: “We will not stop organizing, demanding change or fighting for justice for ourselves and our patients until our system becomes one that promotes well-being both in training and in the delivery of care.”
This article was originally posted on Lincoln Hospital Doctor Trainees Say Harsh Culture Took Toll Before Three Died
Be the first to comment on "Lincoln Hospital Doctor Trainees Say Harsh Culture Took Toll Before Three Died"